Slide 1 of 3 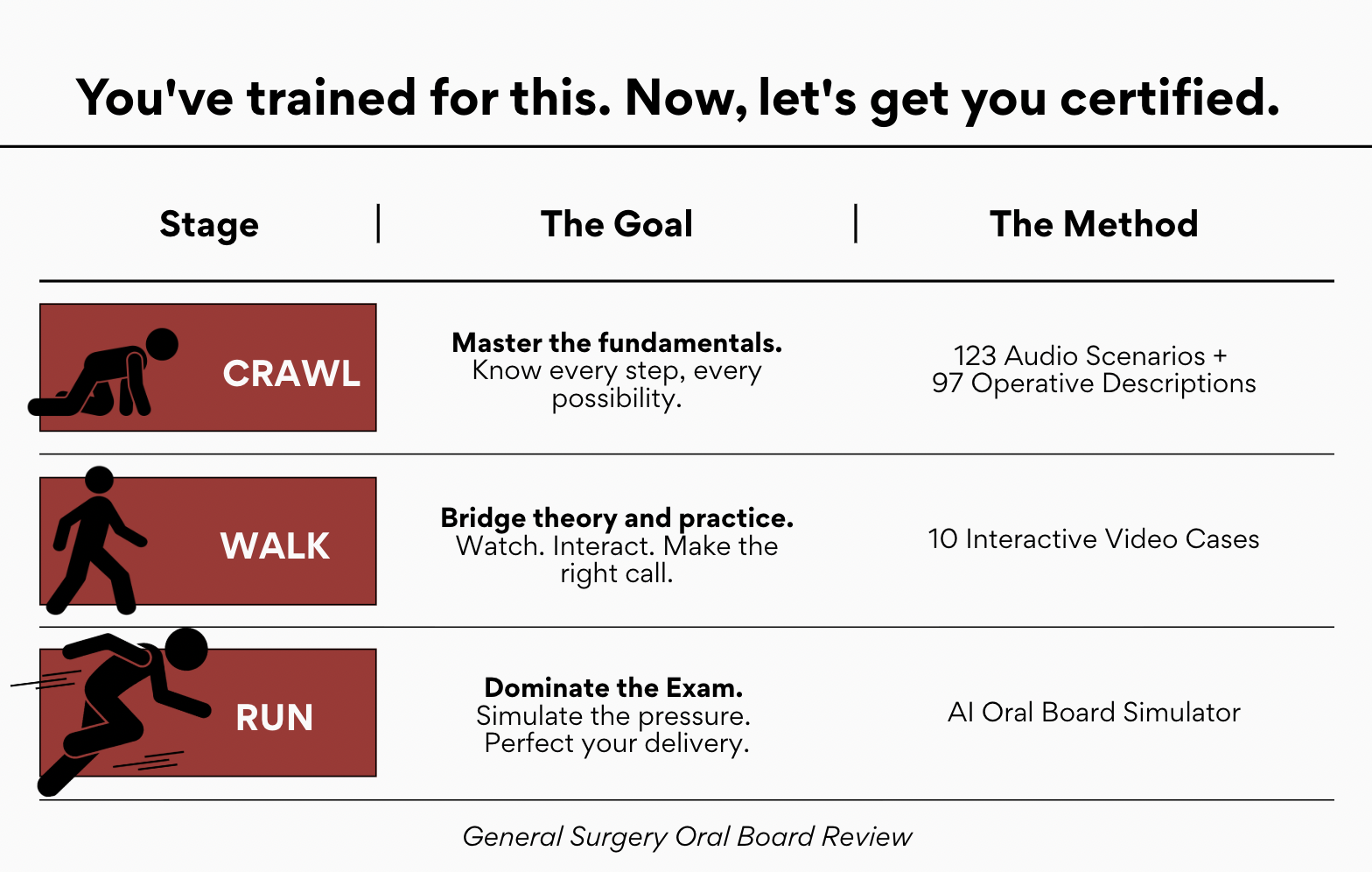
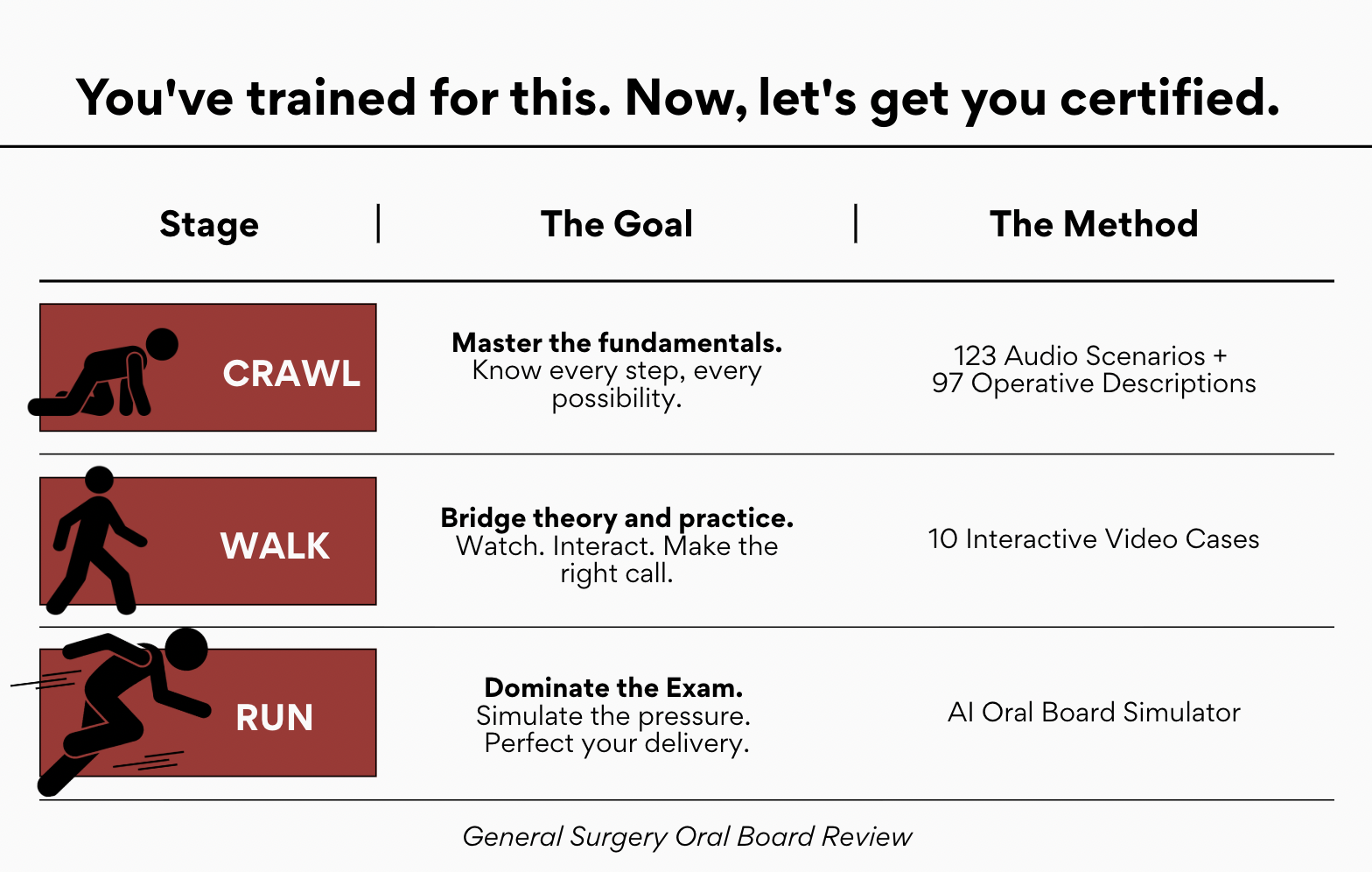
General Surgery Oral Board Review
123 Audio Scenarios + 10 Interactive Video Scenarios + 97 Operative Descriptions + Oral Board Simulator
Slide 2 of 3 
Trauma Surgery Video Atlas
The Trauma Surgery Video Atlas contains 24 scenarios that include never-before-seen high-definition operative footage, rich, original illustrations, and practical, easy-to-read pearls that will help you dominate the most difficult trauma scenarios.

Slide 3 of 3 
Dominate Surgery: A High-Yield Guide to Your Surgery Clerkship
A no-nonsense multimedia resource for students on their surgical rotations.

Latest Podcast Episodes
Recent Videos
Explore Other Topics
AnesthesiaBariatricBreastBurnCareer DevelopmentCOVIDColorectalEmergency General SurgeryEndocrineGeneral SurgeryGlobal SurgeryHepatobiliaryHerniaMinimally InvasiveOrthopedic SurgeryPalliative CarePediatricPlastic SurgeryProceduresSurgical Critical CareSurgical EducationSurgical OncologyTraumaUpper GIVascularConference HighlightsCardiothoracicMiscellaneousMedical StudentHealthcare equitySurgical SkillsTransplantLeadershipRenalSpanishArtificial IntelligenceOBGYN